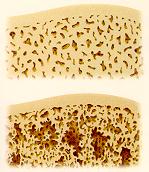
- Normal bone is dense and strong (see top of illustration). Bone with
osteoporosis has thinned out and become more porous, making it more likely
to break (see bottom of illustration).
Osteoporosis is a devastating disease characterized by loss of bone mass that leads to reduced bone strength, poor bone quality and increased risk of fractures. Our bodies continuously break down old bone and rebuild new bone. Osteoporosis is caused by an imbalance in this cycle. During menopause, this cycle is disturbed by hormonal changes - namely, a deficiency of estrogen - which causes women to lose bone faster than it is replaced. And during the first five years after menopause, some women may lose as much as 25% of their bone density. In many women, this bone loss is severe enough to make bones weak and fragile, causing them to break easily.
 |
|
Osteoporosis affects over 20 million American women. More than one in three women over the age of 50 has lost enough bone to put her at increased risk of "fragility" or osteoporotic fractures that can occur at the hip, spine or wrist. It is estimated that as many as 40% of 50 year old women will suffer an osteoporosis-related broken bone at some time during their lives. Broken bones can lead to pain, height loss, difficulty moving around, a deformed backbone that curves forward (sometimes called "dowager’s hump"), and, possibly permanent disability and dependence. The most serious are hip fractures, which usually require hospitalization and often lead to disability and premature death.
Although menopause is the single most important cause of osteoporosis, other factors may add to one’s risk of developing osteoporosis.
As a medical student I was taught that three things were required to keep bones strong and healthy after menopause: calcium, exercise, and last but not least, estrogen replacement. It was and still is widely accepted that this combination will slow or prevent bone loss during a woman’s menopausal years. Prevention was the name of the game since there was no effective treatment for osteoporosis once it had occurred. Today, although calcium, exercise and estrogen remain the best defense against osteoporosis, new drugs are being developed for the treatment of osteoporosis. The newest of these is Fosamax.
Fosamax is the first in a new class of drugs called aminobisphosphonates to treat osteoporosis in postmenopausal women. Fosamax works by reducing the activity of the cells that cause bone loss thereby decreasing the faster rate of bone loss that occurs after menopause and by increasing the amount of bone in most patients. These effects are seen as soon as three months after therapy with Fosamax is begun and continues as long as you are taking Fosamax.
Fosamax has been shown to build healthy bone, reduce the risk of spinal fractures by nearly half and decrease the resulting loss of height. It has been studied in more than 1,800 women in five clinical trials. Data show that, over three years, Fosamax builds healthy bone at the spine and hip and other sites by as much as 10%, compared with patients treated with placebo (an inactive compound) whose bone mineral density decreased. Results of a multinational study show a 48% reduction in the proportion of women who suffered new spinal fractures among patients treated with Fosamax versus patients treated with placebo.
Osteoporosis is a "silent" disease. Because they feel no pain during the early stages of the disease, many women who are careful to get enough calcium and exercise think that osteoporosis is not a real concern. Unfortunately they may have it for years and not find out until they break a bone. Getting diagnosed as early as possible is very important so steps can be taken to help limit bone loss at the earliest possible stage. The diagnosis may be made on the basis of certain signs or symptoms such as back pain, height loss or a curving spine. In the absence of such signs, bone density testing may be warranted especially in women who have multiple risk factors for the development of osteoporosis.
Remember an ounce of prevention is worth a pound of cure. Every woman should consult her physician at the time of menopause regarding her individual risk for osteoporosis. Hormone replacement therapy should be considered as the best preventative medicine for osteoporosis. When the use of estrogen replacement is contraindicated (as in patients with a history of breast cancer) or simply not tolerated, Fosamax may be considered. Fosamax might also be considered in any patient who has signs or symptoms of osteoporosis. Lifestyle changes may also be required. The most useful of these would be to stop smoking, reduce the use of alcohol, exercise regularly and eat a balanced diet with adequate (or supplemented) calcium and vitamin D.
For further information visit the National Osteoporosis Foundation.
Walter J. Hodges Jr., M.D., F.A.C.O.G.